Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pan Z. Histiocytic sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodeshistiocyticsarcoma.html. Accessed December 22nd, 2024.
Definition / general
- Malignant proliferation of cells with morphologic and immunophenotypic features of mature histiocytes, excluding dendritic cell neoplasms, Langerhans cell neoplasms and myeloid sarcomas with monocytic differentiation
- Mostly in extranodal locations, including skin, soft tissue, lung and central nervous system
- A small subset (~17%) in lymph nodes
- Diagnosis requires histopathologic evidence of neoplasm and confirmation of cell origin by special studies
Essential features
- Malignant neoplasm of mature histiocytes
- May show highly pleomorphic or spindle cytology, mimicking pleomorphic or spindle cell sarcoma
- Can be dedifferentiated from B cell lymphomas, myeloid neoplasms and rarely T cell lymphomas
- Positive BRAF V600E mutation and clonal IGH or TRG rearrangements in a subset of cases
Terminology
- Histiocytic medullary reticulosis, malignant histiocytosis, true histiocytic lymphoma, true histiocytic sarcoma
Epidemiology
- < 1% of all hematolymphoid neoplasms (Leuk Lymphoma 2019;60:553)
- Incidence: 0.17 cases per 1,000,000 individuals
- Usually adults, median age ~61 years
- Slight male predilection, M:F = 5:3
Sites
- Mainly extranodal locations, including skin, soft tissue, lung and central nervous system (Leuk Lymphoma 2019;60:553)
- ~17% of cases in lymph nodes
Etiology
- No specific etiologic agents discovered
- ~25% of cases transdifferentiated from B cell lymphomas, including small lymphocytic lymphoma / chronic lymphocytic leukemia, follicular lymphoma, mantle cell lymphoma, extranodal marginal zone lymphoma and diffuse large B cell lymphoma (Hum Pathol 2016;55:39, Eur J Haematol 2016;97:9)
- Rare cases associated with B cell or T cell lymphoblastic lymphoma / acute lymphoblastic leukemia, myeloid neoplasms and mediastinal nonseminomatous germ cell tumors (Lancet Oncol 2004;5:248, Medicine (Baltimore) 2016;95:e2515)
Clinical features
- Mostly advanced diseases with B symptoms (fever, fatigue and weight loss)
- Physical examinations: lymphadenopathy, hepatosplenomegaly and skin lesions
- Lytic bone lesions and rare central nervous system involvement
- Median overall survival, 6 months (Leuk Lymphoma 2019;60:553)
Diagnosis
- Presence of mature histiocytic cytology with variable degree of pleomorphism
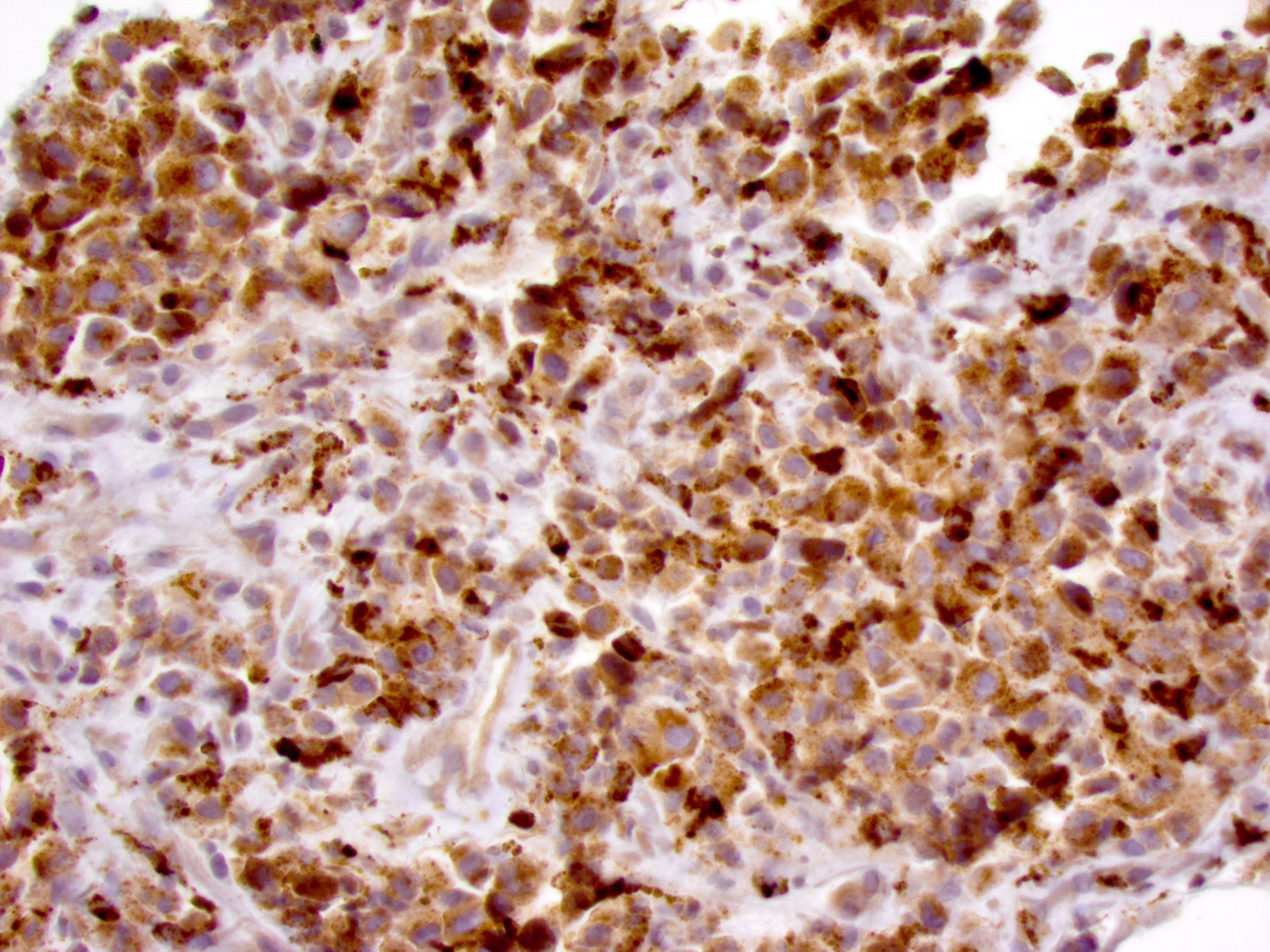
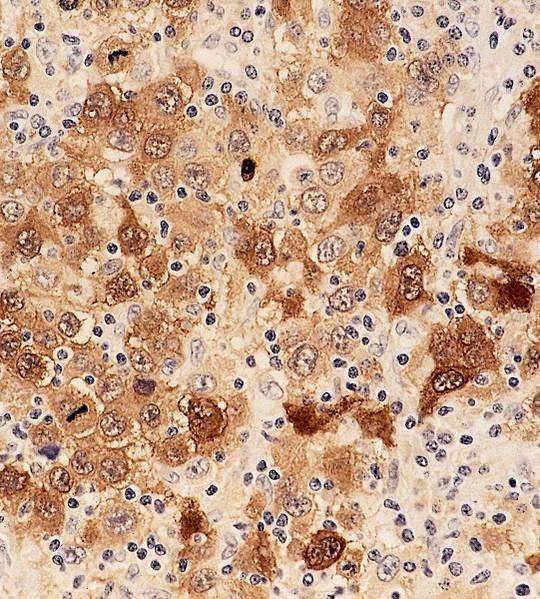
- Positive for histiocytic markers, particularly CD68, CD163 and lysozyme
- Exclusion of myeloid sarcoma with monocytic differentiation, Langerhans cell neoplasm and other mimicries
Prognostic factors
- Surgery alone or in combination with radiotherapy was associated with a prolonged overall survival in patients with skin and connective tissue disease (Leuk Lymphoma 2019;60:553)
- Surgical treatment showed some statistically insignificant improvement in overall survival in patients with gastrointestinal and lung disease
- Patients with hematopoietic and reticuloendothelial system involvement had a poor prognosis even with systemic chemotherapy
- Compared with de novo cases, secondary histiocytic sarcomas have a more aggressive course and shorter overall survival (Clin Lymphoma Myeloma Leuk 2018;18:e427)
Case reports
- 47 year old woman with primary central nervous system histiocytic sarcoma with PDGFR mutation and PDL1 / PDL2 expression (Radiat Oncol 2018;13:167)
- 50 year old African American woman with clonally related histiocytic sarcoma and B lymphoblastic leukemia / lymphoma (Am J Clin Pathol 2019;152:486)
- 63 year old white woman with histiocytic sarcoma associated with splenic marginal zone lymphoma (J Med Case Rep 2017;11:92)
- 72 year old man with histiocytic sarcoma secondary to chronic myeloid leukemia (Eur J Haematol 2016;97:9)
- 74 year old man with histiocytic sarcoma arising from hairy cell leukemia (J Clin Oncol 2014;32:e117)
- 75 year old man with histiocytic sarcoma associated with follicular lymphoma (Clin Lymphoma Myeloma Leuk 2019;19:e1)
Treatment
- Localized unifocal disease: surgical resection if possible, followed by adjuvant radiotherapy and chemotherapy
- Disseminated disease: more intense chemotherapy regimens, including ifosfamide, carboplatin and etoposide; CHOP-like (cyclophosphamide, doxorubicin, vincristine and prednisone) chemotherapy; autologous hematopoietic stem cell transplantation (Clin Lymphoma Myeloma Leuk 2019;19:522)
- Central nervous system cases: surgery, chemotherapy and focal radiation (Radiat Oncol 2018;13:167, Leuk Lymphoma 2016;57:1961)
- Cases with activated RAS / MEK / ERK pathway: MEK inhibitor, trametinib (Int J Hematol 2019;109:228)
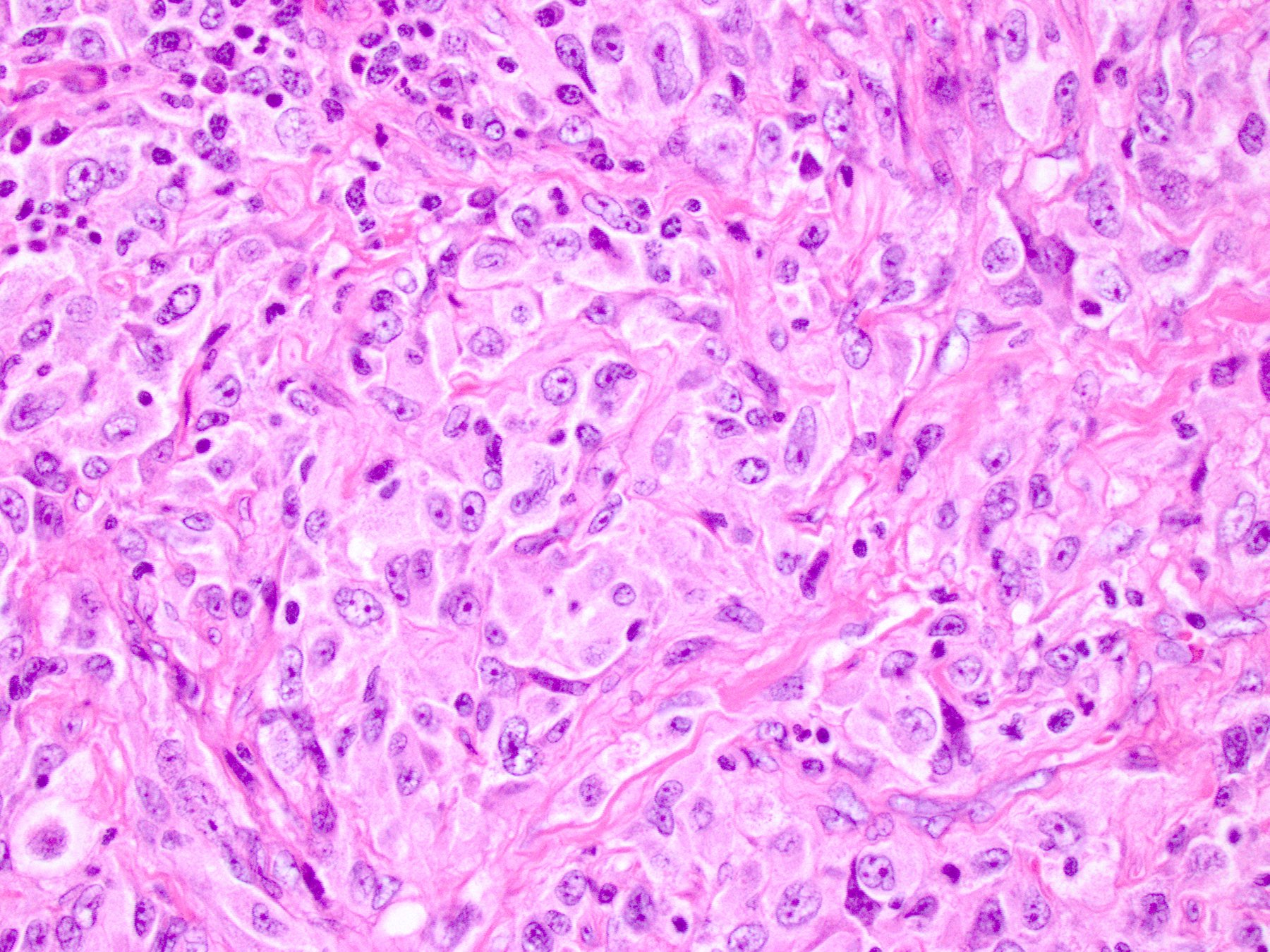
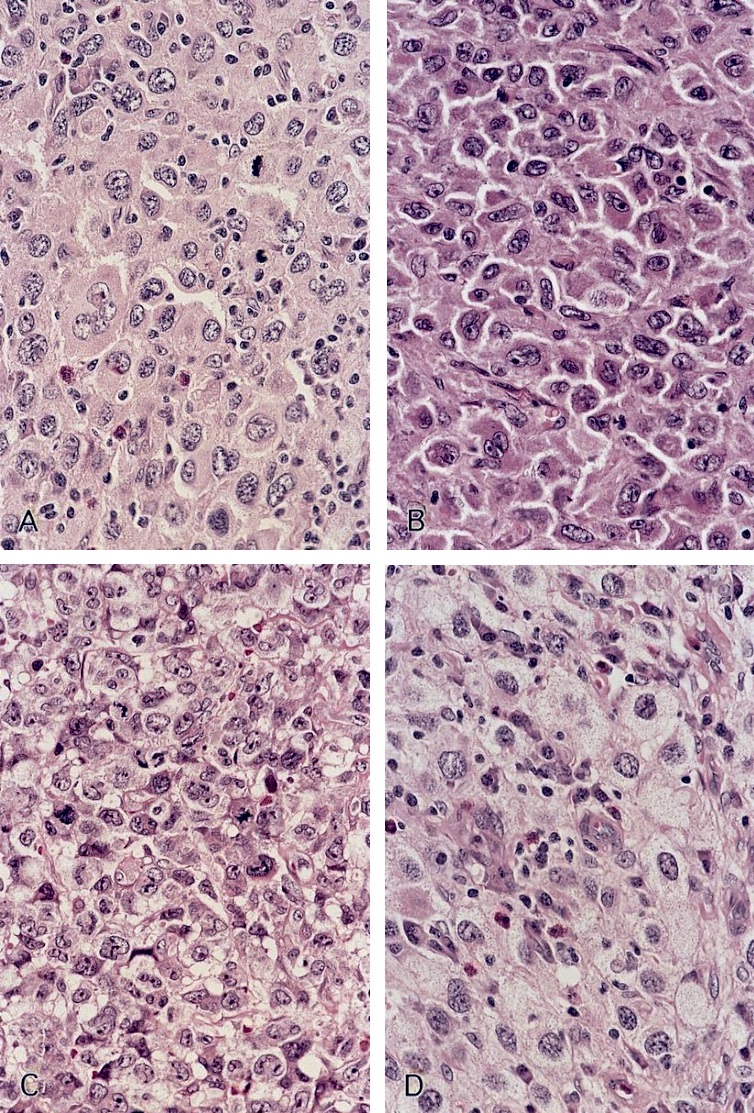
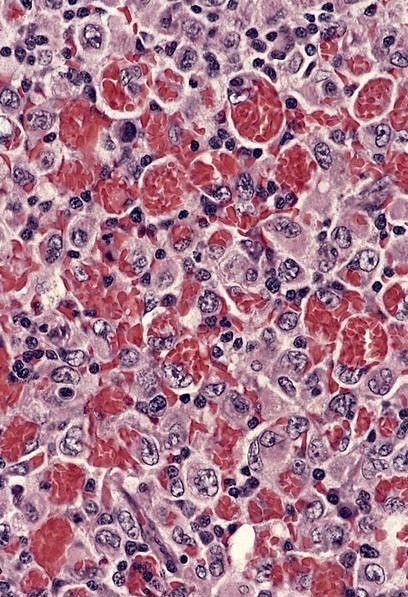
Microscopic (histologic) description
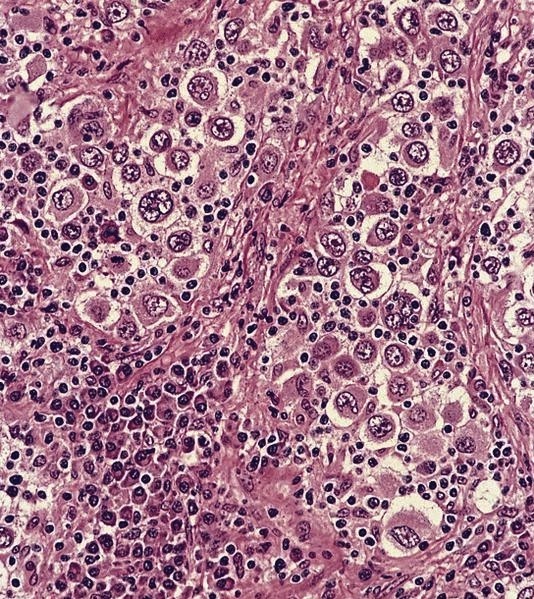
- Diffuse infiltration in the soft tissue or characteristic sinusoidal infiltration in the lymph nodes, liver and spleen
- Effacement of nodal architecture or commonly sinus expansion with sparing of follicles
- Large tumor cells with variable pleomorphism but often resembling mature histiocytes
- Oval or irregular and eccentrically placed nuclei with vesicular chromatin, large nucleoli and occasional grooves
- Abundant eosinophilic cytoplasm, often foamy or vacuolated
- Rarely with multinucleated giant tumor cells, erythrophagocytosis or focal spindling cytology
- Increased mitotic figures and apoptotic cells and presence of tumor necrosis
- Mixed inflammatory background with variable numbers of reactive lymphocytes, plasma cells, benign histiocytes and eosinophils
- Reference: Surg Pathol Clin 2019;12:805
Microscopic (histologic) images
Positive stains
Negative stains
- B cell and T cell markers
- Follicular dendritic markers: CD21, CD23 and CD35
- Langerhans cell markers: CD1a and CD207
- S100 typically negative albeit focal reactivity in some cases
- CD34, CD30, HMB45, myeloperoxidase and cytokeratins
- Reference: Surg Pathol Clin 2019;12:805
Electron microscopy description
- Abundant surface activity, microfilaments, short segments of rough endoplasmic reticulum, scattered haloed granules
- No Birbeck granules
- Reference: Surg Pathol Clin 2019;12:805
Molecular / cytogenetics description
- Clonal IGH and TRG rearrangements in a subset of bona fide cases and cases dedifferentiated from lymphomas (Oncotarget 2016;7:78355)
- Cases transdifferentiated from B cell lymphomas retain the same genetic alterations in the prior B cell lymphoma, including t(14;18) in follicular lymphoma and del(13q) in small lymphocytic lymphoma / chronic lymphocytic leukemia (Diagn Cytopathol 2015;43:659)
- BRAF V600E mutation detected in up to 63% of cases (Histopathology 2014;65:261)
- Rare cases associated with mediastinal nonseminomatous germ cell tumors harbor isochromosome 12p (Medicine (Baltimore) 2016;95:e2515)
Sample pathology report
- Lung, right upper lobe, wedge biopsy:
- Histiocytic sarcoma, dedifferentiated from follicular lymphoma (see comment)
- Comment: The patient had a history of follicular lymphoma (grade 1 - 2 of 3) 3 years ago, and the current pulmonary histiocytic sarcoma demonstrates IGH-BCL2 rearrangement by FISH studies and clonal IGH rearrangements by PCR assays. Therefore, this histiocytic sarcoma represents dedifferentiation from previous follicular lymphoma, which has been reported in the literature (Leukemia 2014;28:1937).
- Microscopic description: The wedge biopsy reveals a diffuse infiltrate of large, pleomorphic cells. The tumor cells have round or irregular nuclei, vesicular chromatin and prominent nucleoli. The cytoplasm is abundant and pale staining. Frequent mitotic figures and apoptotic cells are noted. No small lymphoma cells are present within the specimen.
- Immunohistochemical stains: The large tumor cells are diffusely positive for CD45, CD68, CD163 and lysozyme. S100 only stains a small subset of cells. All other markers studied are negative, including CD1a, CD3, CD20, cytokeratins (AE1 / AE3, CK7 and CK20) and melanocytic markers (SOX10, HMB45 and MelanA).
- Flow cytometric assays: No evidence of monotypic B cell or abnormal T cell population detected.
- FISH studies: Positive for IGH-BCL2 gene rearrangements in 47% of 200 cells analyzed.
- Molecular studies: Positive for clonal IGH gene rearrangement. Negative for clonal TRG gene rearrangement.
Differential diagnosis
- Diffuse large cell lymphoma:
- Anaplastic large cell lymphoma:
- Rosai-Dorfman disease:
- Langerhans cell histiocytosis:
- Metastatic carcinoma with anaplastic features:
- Clinical history of carcinoma
- Positive for cytokeratin
- Metastatic melanoma:
- Myeloid sarcomas with monocytic differentiation:
- Reactive histiocytosis and storage diseases:
- May present with a marked histiocytic infiltration in the sinuses
- Lack of significant cytologic atypia
Additional references
Board review style question #1
Which of the following immunohistochemical stains are mostly positive in histiocytic sarcoma?
- CD4, CD1a, S100
- CD21, CD23, CD35
- CD34, myeloperoxidase, CD117
- CD45, CD68, CD163
Board review style answer #1
Board review style question #2
Which of the following statements is true regarding histiocytic sarcoma?
- Cases dedifferentiated from B cell lymphomas usually retain the expression of B cell markers
- Clonal IGH or TRG rearrangements detected in a subset of cases
- Most cases initially occur in the lymph nodes
- Typically expresses CD68, S100 and CD1a
Board review style answer #2
B. Clonal IGH or TRG rearrangements detected in a subset of cases
Comment Here
Reference: Histiocytic sarcoma
Comment Here
Reference: Histiocytic sarcoma